
Traditional Birth Attendants (TBA) are an important piece in Uganda’s maternity care puzzle. They fill a crucial staffing gap in the formal healthcare system and are uniquely placed to establish positive relationships with the wider community. But the Ugandan government, keen to promote “modern” birth practices, has outlawed the use of TBAs. This article argues for a new approach: integrating TBAs into the state healthcare system, tapping on their expertise and knowledge of local herbal resources for the benefit of the wider community.

In order to reduce maternal mortality, in 2010 the government of Uganda outlawed the use of traditional birth attendants in conducting childbirths, encouraging mothers to give birth in recognized “modern health facilities.” While this may appear to be the ideal situation for childbirth, there are many structural and healthcare delivery system challenges that are hindering this policy. On the one hand, there is a lack of adequate government support for modern health units; on the other, mothers in rural areas have continued to seek the services of traditional birth attendants, who are significant in community life despite government intervention. Appreciating and supporting the work of traditional birth attendants in providing maternal health care in low-resource remote communities, rather than outlawing them, is as important as promoting birth through “modern” birth practices. In this article, we highlight the challenges associated with outlawing traditional birth practices and the opportunities that the use of traditional birth attendants create, to argue that the government of Uganda should strike a balance between traditional and “modern” birth practices in the promotion of maternal health care and the reduction of maternal mortality in low-resource remote communities. Such a balance will ensure the effective regulation of the traditional birth delivery sector, while at the same time helping to build trust between the government and other stakeholders in the sector.
The World Health Organization (WHO) defines traditional birth attendants as persons who assist a woman during childbirth and who initially acquired their skills by delivering babies themselves or through an apprenticeship to other traditional birth attendants. In Uganda, traditional birth attendants (TBAs) have historically been the principal caregivers for women during childbirth and throughout the antenatal period. While they may not have undergone formal training, in a sector where the experience of a health practitioner can sometimes be the difference between life and death, these traditional midwives have over the years offered invaluable advice and support before, during, and after pregnancy. They are a repository of local herbal knowledge, which they use to prescribe herbs that aid women during and after childbirth.
The Ministry of Health of Uganda (2020) has reported that 416,000 of 1.5 million women do not seek a skilled “modern midwife,” and resort to TBA for the delivery of their children. This figure might be an underestimate, because it only accounts for the brave women who choose to register the birth of their children at sub-county health centers, despite the risk of legal sanctions because they gave birth with the support of an outlawed traditional birth attendant.
Studies in Uganda have shown that traditional birth attendants are sought out by pregnant women because they are cheap, easily accessible at all hours, affordable, and culturally acceptable—the last because they usually share similar cultural and religious beliefs, which is not the case with western-trained midwives. The pregnant women further believe that the care provided by traditional birth attendants is excellent, with a smaller likelihood of having to undergo a C-section. They also feel more secure with traditional birth attendants than with western-trained midwives because the herbs provided by traditional birth attendants reduce the labor period. Pregnant women also argue that maternal mortalities occur both in modern health facilities and with traditional birth attendants.
“We argue that Uganda should strike a balance between traditional and modern medical practices. One example is the training and skilling of traditional birth attendants, which would provide a good basis for harmonizing indigenous and modern knowledge in maternity care.”
These arguments put forward by mothers in Uganda may not be sufficient to rationalize the use of traditional birth attendants. But if considered within the context of the state of health facilities in Uganda, one can begin to understand why mothers seek out traditional birth attendants. Uganda’s public health system is organized in seven tiers: national and regional referral hospitals, general district hospitals, and four levels of health centers (HCs), at the community (HC1), parish (HC2), sub-county (HC3), and county (HC4) levels, as seen below.
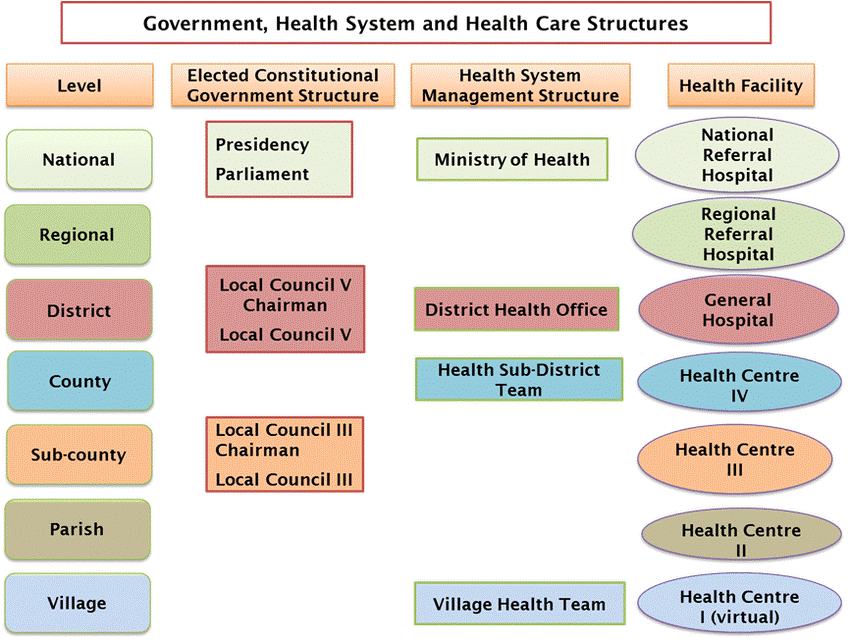
Staffing and available services vary across the four levels. HC3 and HC4 offer Emergency Obstetrics Care (EMOC), whereas HC1 and HC2 serve as low-resource referral units, unable to provide EMOC and without ambulances or blood transfusion services. The national and regional referral hospitals, as well as the district hospitals and health centers (4), which seems to be equipped with quality medical equipment, are very far from the remote regions of Uganda and lack essential drugs. This is coupled with a chronic shortage of trained health workers. For example, only 38% of healthcare posts in Uganda are filled. Health workers in the country have little incentive to work in poor rural areas. Some 70% of Ugandan doctors and 40% of nurses and midwives are based in urban areas, serving only 12% of the Ugandan population. On the other hand, the third, second, and first tier health centers ( (HC 3, 2, & 1), which are meant to serve under-resourced remote communities, are under-staffed, struggle to attract health care workers, do not provide EMOC, and have no ambulances or blood transfusion services. All the above make the traditional birth attendant the best option in remote communities in Uganda.
Therefore, outlawing traditional TBAs in the low-resource villages means that TBAs operate illegally and are not supported by the government. Their services continue to be vaguely regarded as a type of informal support; there is no clear guidance on how they should be incorporated into the formal health practice, or on the legal basis for their operation, yet they continue to provide services to many pregnant women. While we acknowledge that the risk involved in giving birth with traditional birth attendants may be high, outlawing or banning their services and criminalizing them may not be the right thing to do in under-resourced remote communities, as it exposes pregnant women to a greater risk of maternal mortality.
We argue that Uganda should strike a balance between traditional and modern medical practices. One example is the training and skilling of traditional birth attendants, which would provide a good basis for harmonizing indigenous and modern knowledge in maternity care. In remote communities, traditional birth attendants should be employed to bridge the healthcare manpower gap, especially in non-technical but critical areas such as building effective referral systems. Here, TBAs can link mothers to qualified birth attendants and provide ante-natal and post-natal counseling. In the end, the skilled birth attendants will attend the delivery of babies, while the TBA will mobilize, counsel, and follow up on mothers. The trust that the community has towards TBAs can be utilized in this arrangement.
Solomon Mbubi
A 2019 Glocal graduate. Formerly he worked as Uganda's Programs Manager for IsraAID, today he is working as an East Africa Programs Manager for HORIZONT3000 — an Austrian Agency for International Cooperation.
Alphonse Chefor Akouyu.
A 2019 Glocal Graduate. He is currently based at the Secretariat of the Regional Network of Agricultural Policy Research Institutes (ReNAPRI) where he works as an Assistant Program Coordinator. His previous experience includes working in various development agencies across Africa. Alphonse is eternally grateful for the scholarship opportunity from the Glocal program which enabled him to acquire the skills needed to work in international development.


